PD-L1xVEGF Bispecific: 1st Global Data from BioNTech/BMS

PD-L1xVEGF Bispecific: 1st Global Data from BioNTech/BMS
The oncology world is buzzing with the release of the first-ever global clinical data for a novel pd-l1xvegf bispecific antibody developed in collaboration by BioNTech and Bristol Myers Squibb (BMS). The results from the Phase 1/2 trial, presented at a major oncology conference, suggest a promising new avenue for treating advanced solid tumors that have been resistant to current therapies.
This innovative drug, known as acasunlimab (BMS-986442 / BNT327), is designed to simultaneously block two critical pathways involved in tumor growth and immune evasion. The initial findings offer a glimpse into its potential efficacy and safety, marking a significant milestone for this class of next-generation immunotherapies.
Table of Contents
What is a PD-L1xVEGF Bispecific Antibody?
To understand the excitement, it’s essential to break down the drug’s dual-action mechanism. A bispecific antibody is an engineered protein that can bind to two different targets at the same time. In this case, the targets are:
- PD-L1 (Programmed Death-Ligand 1): This is a protein found on the surface of many cancer cells. It acts as a “stop sign” for the immune system, binding to the PD-1 receptor on T-cells (a type of immune cell) and preventing them from attacking the tumor. Blocking PD-L1 essentially “releases the brakes” on the immune system, a strategy successfully used by checkpoint inhibitors like nivolumab and pembrolizumab.
- VEGF (Vascular Endothelial Growth Factor): This protein is a key driver of angiogenesis, the process by which tumors create new blood vessels to supply themselves with oxygen and nutrients. High levels of VEGF are associated with aggressive tumor growth and metastasis. Anti-VEGF therapies starve the tumor by cutting off its blood supply.
By combining these two functions into a single molecule, the pd-l1xvegf bispecific antibody aims to deliver a powerful one-two punch. It simultaneously boosts the anti-tumor immune response while disrupting the tumor’s nutrient supply chain. Researchers theorize this synergistic approach could be more effective than administering two separate drugs and may even overcome resistance to single-agent therapies.
Key Findings from the Phase 1/2 Trial Data
The Phase 1/2 study (NCT04543722) was designed to evaluate the safety, tolerability, and preliminary efficacy of acasunlimab in patients with advanced solid tumors who had exhausted standard treatment options. The initial data readout included patients with several cancer types, most notably non-small cell lung cancer (NSCLC) and renal cell carcinoma (RCC).
The results were encouraging, particularly in patients who had previously progressed on PD-1/PD-L1 inhibitors.
Efficacy Highlights:
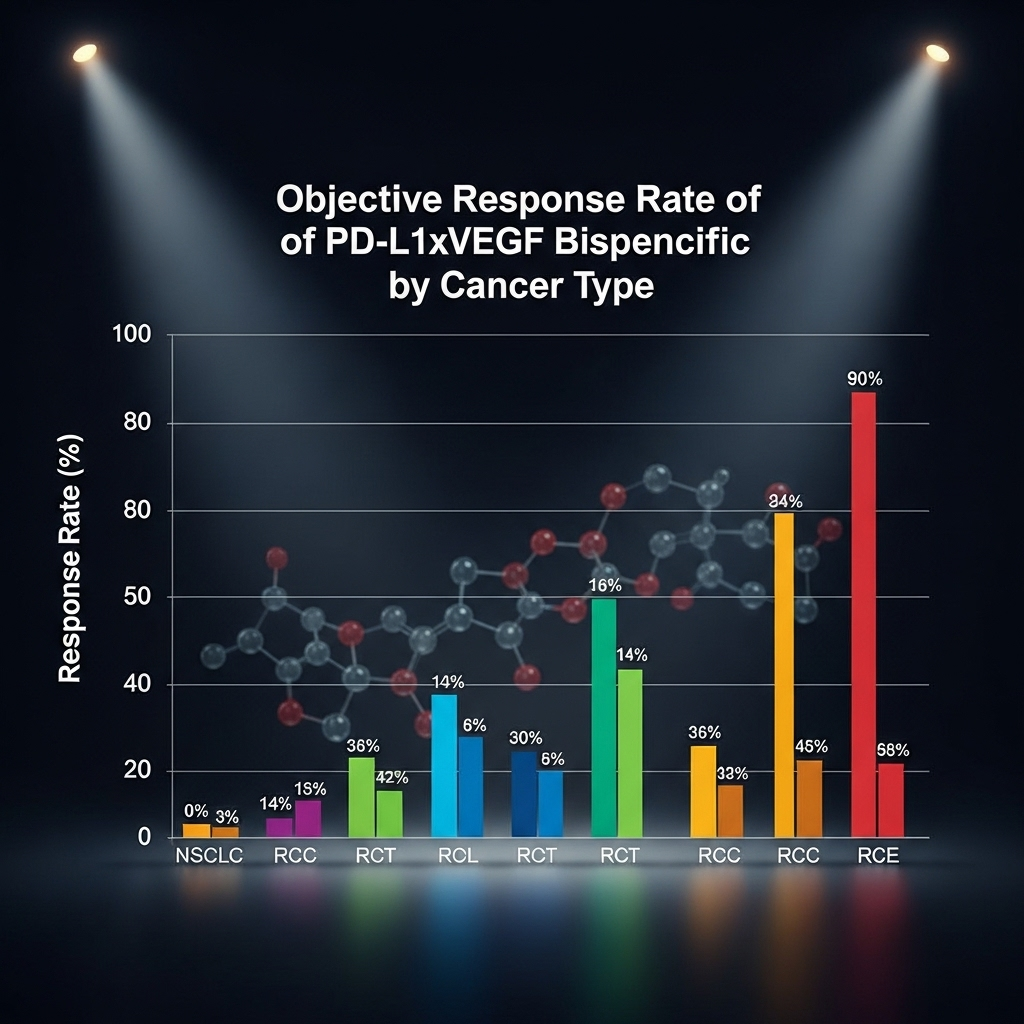
- The overall Objective Response Rate (ORR) across all evaluated tumor types was 29.5%. This is a significant figure for a heavily pre-treated patient population.
- In a cohort of post-checkpoint inhibitor NSCLC patients, the ORR reached 34.1%, suggesting the drug may re-sensitize tumors to immunotherapy.
- The Disease Control Rate (DCR), which includes patients with stable disease, was an impressive 72.3%, indicating that the drug successfully halted tumor progression in a majority of patients for a period of time.
- Median duration of response (DoR) had not yet been reached in several cohorts, pointing towards the potential for durable, long-lasting clinical benefit.
These figures, while preliminary, showcase the potential of this novel approach. The ability to generate responses in patients who have already failed standard immunotherapy is a critical unmet need in oncology today.
Analyzing the Safety Profile of the PD-L1xVEGF Bispecific
With any new therapeutic, especially one with a dual mechanism, the safety profile is paramount. The data presented by BioNTech and Bristol Myers Squibb indicated a manageable safety profile consistent with the known effects of blocking the PD-L1 and VEGF pathways individually.
The most common treatment-related adverse events (TRAEs) were generally low-grade and included:
- Hypertension: A known side effect of anti-VEGF agents.
- Fatigue: Common with immunotherapies.
- Proteinuria (protein in the urine): Another on-target effect of VEGF inhibition.
- Infusion-related reactions: Generally mild and manageable with standard care.
The rate of Grade 3 or higher TRAEs was reported at 15.8%, a figure that investigators described as acceptable and manageable in this advanced cancer setting. Importantly, there were no new or unexpected safety signals, which provides confidence for moving into later-stage clinical trials. A full breakdown of the data is expected to be published in a peer-reviewed journal like The Lancet Oncology in the coming months.
Implications and Future Directions
The successful first data readout for this pd-l1xvegf bispecific antibody is a significant step forward for several reasons. It validates the scientific rationale of co-targeting these two pathways and establishes a new potential pillar of treatment in cancer research.
Key Takeaways:
- Overcoming Resistance: The most exciting finding is the activity in patients who have already failed checkpoint inhibitors. This suggests a potential to reverse or bypass common resistance mechanisms.
- Broad Potential: While early data focused on specific cancers, the fundamental roles of PD-L1 and VEGF in many tumor types suggest this drug could have broad applicability across oncology.
- Strong Partnership: The collaboration between BioNTech’s innovative research engine and BMS’s deep expertise in oncology development creates a powerful force to advance this molecule rapidly.
The next steps will be critical. BioNTech and BMS have indicated plans to expand the current trial and are likely designing pivotal Phase 3 studies. These trials will aim to confirm the efficacy of acasunlimab against current standards of care in specific patient populations, such as second-line NSCLC or advanced RCC. Further research will also explore potential predictive biomarkers to identify which patients are most likely to respond.
In conclusion, the first global data for the BioNTech/BMS pd-l1xvegf bispecific antibody represents a promising development in the fight against advanced cancer. While it is still early days, the combination of a sound scientific mechanism, encouraging preliminary efficacy, and a manageable safety profile has positioned acasunlimab as a molecule to watch closely in the evolving landscape of cancer therapy.
“`